Several months after discreetly acquiring the online prescription service HeyDoctor, GoodRx is launching a new service based on the acquisition, GoodRx Care and offering a direct challenge to online prescription services like Hims, Hers, Nurx, Ro and others.
Already a billion-dollar giant in the world of prescription fulfillment through its cost-comparison and discount medication fulfillment business, more than 10 million consumers use the company’s services already.
With GoodRx Care, customers can use the online medical service to get a consultation, treatment, prescriptions and lab tests from doctors. The array of services on offer, which covers conditions and ailments from urinary tract infection treatments and birth control pills to erectile dysfunction medication and hair replacement supplements, mirror those pitched by white-glove online prescription services like Ro, Hims, Hers, and Nurx .
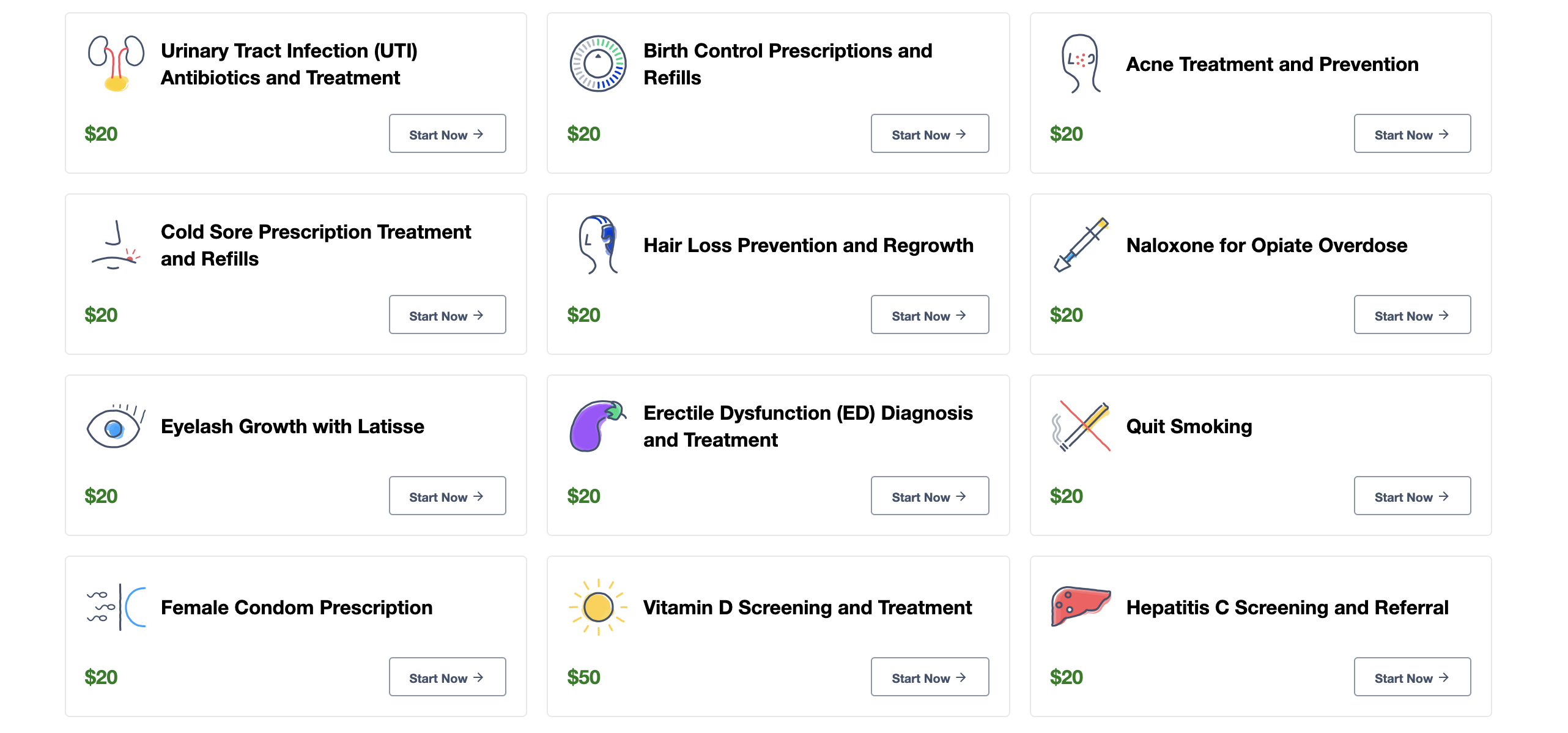
GoodRx Care services
“Over the years, we’ve helped millions of Americans find affordable solutions for their prescription medications, but have also learned that many people struggle to get to the doctor,” said Doug Hirsch, co-CEO and co-founder of GoodRx. “By introducing GoodRx Care, we aim to help fill in the gaps in care to improve access, adherence, and affordability of medical care for all Americans.”
For Hirsch and GoodRx, the expansion into these kinds of online consultations was a natural extension of the company’s services. “One third of people who come to GoodRx . are coming to GoodRx and they may not have the prescription that they don’t think they need,” he says. “For a long time now we’ve been telling people you may need a prescription for the service and telemedicine options are available.”
Now the company can keep those customers in-house by offering their own telemedicine consults.
Other technology companies are also pushing deeper into the healthcare industry with Amazon making a big splash with the launch of its employee-only healthcare service offering telemedicine and on-site consultations with staff doctors. Apple, too, has its own healthcare service for employees.
Even BestBuy is seeing big dollars in the healthcare industry. It expects healthcare services to become an increasingly important component to its bottom line as more technology hardware and software is developed to cater to both the aging population, remote health solutions, and infant and childcare.
Demand for more healthcare alternatives is only increasing even as the cost of care rises and the value of healthcare services declines.
As GoodRx notes, access to primary care physicians is hard for most Americans. Some patients can wait up to three weeks to see a doctor and there’s the potential that the country could see a shortfall of up to 120,000 doctors coming within the next 15 years. Add that to the fact that over 27.5 million Americans don’t even have health insurance and the demand for low cost access to care seems obvious.
What’s less obvious is that the care Americans need is access to physicians which will prescribe hair-loss or erectile dysfunction treatments, acne treatments, eyelash growth, or metabolic assessments.
Hirsch says more services will be coming in later months. “We’re at the very early stages of telemedicine,” he says. “We want to continue to expand into more primary services as is safe and affordable and as we can.”
For now, the focus was on bringing the price point down and having more control over where to refer customers. “A lot of these services are tied to mail-order clinics and that could be hundreds of dollars [for a consultation or prescription],” Hirsch says. “We’re going to say it’s $20 for a visit. You can do it today… and you can have a pricing options… we’re saying you’ve had your doctor visit… here’s a list of prices and coupons if you want them.”
Since its launch in 2017, HeyDoctor has had over 100,000 consultations and had already been working with GoodRx, according to Hirsch. The terms of the acquisition were not disclosed.
The acquisition of HeyDoctor is the first big strategic gambit from the company in the year since it raised money from the private equity firm, Silverlake, in a transaction which valued the discount pharmaceutical provider at roughly $2.8 billion, according to a CNBC report.
“In an increasingly fragmented and confusing healthcare system, our goal is to provide a one-stop shop for services that address most basic healthcare needs,” said Hirsch.